Fast Facts about Cavernoma
With over 3500 members in the UK and worldwide, the charity aims to raise awareness of this relatively unknown condition throughout the general public as well as the medical community.
Below we present a series of quick facts about cavernoma, and how it may impact a person.
Fast Facts
- Cavernoma are also known as Cavernous Angioma and Cerebral Cavernous Malformation (CCM).
- A cavernoma is a raspberry-shaped abnormal blood vessel (blood capillary) with thin, leaky walls.
- Cavernoma are found mostly in the brain and spinal cord.
- A cavernoma is neither a tumour nor a compression, but a malformation of blood vessels.
- Most people will have no symptoms – these are known as asymptomatic cavernoma. Research figures vary, but it is thought that about 1 in 625 people has an asymptomatic cavernoma.
- Cavernoma can become symptomatic at any age, most commonly when a person is between the ages of 20-40. Again, research figures vary but it is thought that only about 160 people in the UK are diagnosed with symptomatic cavernoma each year.
- Cavernoma can grow and hemorrhage (bleed) at any age, including in young children, when the symptoms normally become more severe.
- The most common first symptom is seizure (50%), followed by hemorrhage (25%) and neurological deficits (25%) like blurred vision and weakness in limbs.
- Cavernoma are hereditary in about 20% of people who have the condition, according to the rare disease resource Orphanet. These are known as familial cavernoma and tend to form at an earlier age.
- Those with the hereditary form will probably have more than one cavernoma and will develop more over time. Those with the non-hereditary form (known as sporadic cavernoma) normally have just one cavernoma.
- The hereditary form can be caused by a mutation on any one of three genes: CCM1, CCM2, and CCM3.
- The hereditary (familial) form of cavernoma does not skip generations. Each child of an affected person has a 50/50 chance of inheriting cavernoma.
- Treatment of cavernoma is often to just treat the symptoms (e.g. with anti-epileptic drugs for seizures and epilepsy).However, if the symptoms are severe, or if the risk of a bleed is considered high, then a clinician may recommend either surgery to remove the cavernoma or what is known as stereotactic radiosurgery to zap it with radiation.
Below is a a diagram of a patient with a temporal lobe cavernoma.
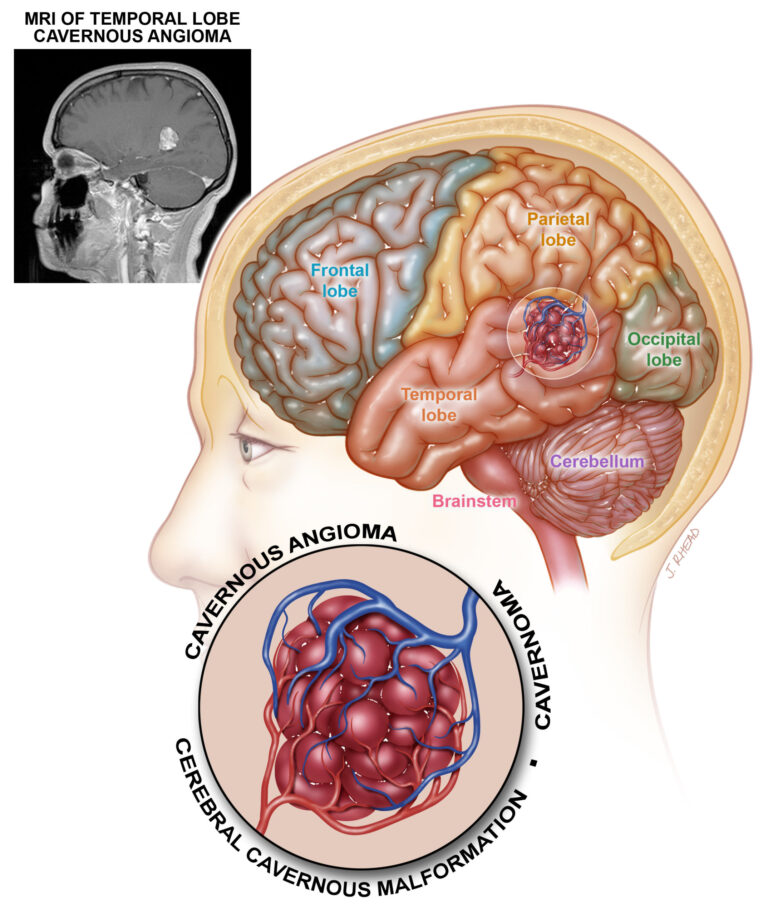
The diagram is reproduced, with permission, from Angioma Alliance. These “Fast Facts” are based on a similar set to be found on the Angioma Alliance website, edited and adapted for the UK.
For more information please see https://www.angioma.org/newly-diagnosed/fast-facts/
For emotional and practical support please contact us, please see our contact page
